Medicare’s effort to reward hospitals for quality is leaving many of the nation’s safety-net hospitals poorer, a new analysis finds.
Dr. Ashish K. Jha, a professor at the Harvard School of Public Health, has found that hospitals treating the most low-income patients on average had their payment rates reduced by 0.09 percent in the latest round of Medicare’s program that rates hospitals’ quality. The hospitals with the fewest low-income patients received an average bonus of 0.6 percent. Government-owned hospitals in particular fared poorly, with Medicare reducing their payment rates by 0.10 percent for a year, according to Jha’s analysis, which he published Tuesday on his Harvard blog.
Medicare bases its bonuses and penalties, created by the federal health care law, on 24 quality measurements, including how patients rated hospitals in surveys and on mortality rates. In the second year of the program, which stretches from last month through September 2014, Medicare has reduced payments to 1,451 hospitals and increased payments to 1,231 hospitals based on those scores. During that period, Medicare will distribute $1.1 billion in the program, known as Value-Based Purchasing, with bonuses going to hospitals that either have better quality than most or that have improved their scores more than most.
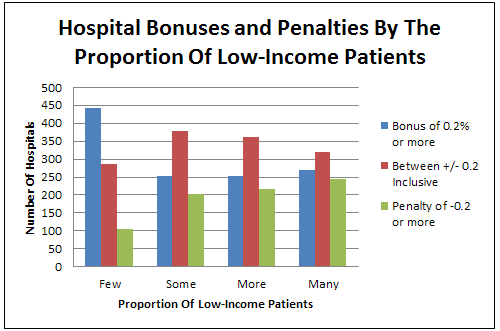
A Kaiser Health News analysis of this year’s financial incentives shows that while safety-net hospitals as a group had larger penalties than other types of hospitals, 32 percent of safety-net hospitals fared well, earning bonuses of at least 0.2 percent, while 29 percent were given penalties of 0.2 percent or more.
But the group of hospitals with the fewest low-income patients did significantly better: 53 percent earned bonuses of 0.2 percent or more. Only 13 percent of these hospitals lost 0.2 percent or more, the KHN analysis found.
Medicare argues that the fact that some safety-net hospitals excel in these kinds of quality programs shows they get a fair shot. In a recent interview, Dr. Patrick Conway, Medicare’s chief medical officer, said that the incentive programs have led to improvements in the quality of four of five hospitals. Because the Value-Based Purchasing program pits hospitals against each other in a competition for money, there will always be about half of hospitals losing funds each year.
While the program’s penalties are not gigantic, the poorer performance of safety-net hospitals nonetheless bolsters concerns that efforts to link pay to performance may increase the gap between well-heeled hospitals that treat affluent patients and safety-net hospitals, many of which struggle to stay financially viable. This has been a significant concern with Medicare’s penalties for hospitals with frequent readmissions, leading Congress’ Medicare Payment Advisory Commission to recommend changes in the way the penalties are assessed.
In a blog post, Jha said it was not clear why safety-net hospitals are falling behind in the value-based purchasing program.
“My suspicion is that much of the difference is driven by differences in patient experience scores. The challenge for all of us is to understand why safety-net hospitals generally have worse patient experience scores. Is it that poorer or minority patients are just less likely to give high scores on patient experience? Or are safety-net hospitals not doing as good of a job on patient-centered care? Until we know, we must be careful declaring that this is an unfair playing field.”
Jha also found a “moderate” regional difference in how all hospitals fared, with those in the Northeast and West doing worse than those in the Midwest and South. Western hospitals lost an average of 0.10 percent of reimbursements and Northeastern ones lost 0.06 percent, while the Midwest gained 0.01 percent and the South lost 0.01 percent. Other factors, such as whether the hospital is large or small or whether it teaches medical residents, did not seem to be linked to higher or lower penalties, Jha found.
To see the financial incentives for specific hospitals, go to Kaiser Health News’ interactive chart or see a summary of how hospitals in each state did.